




Author: Dr. Garima Biswas
Yoga 0
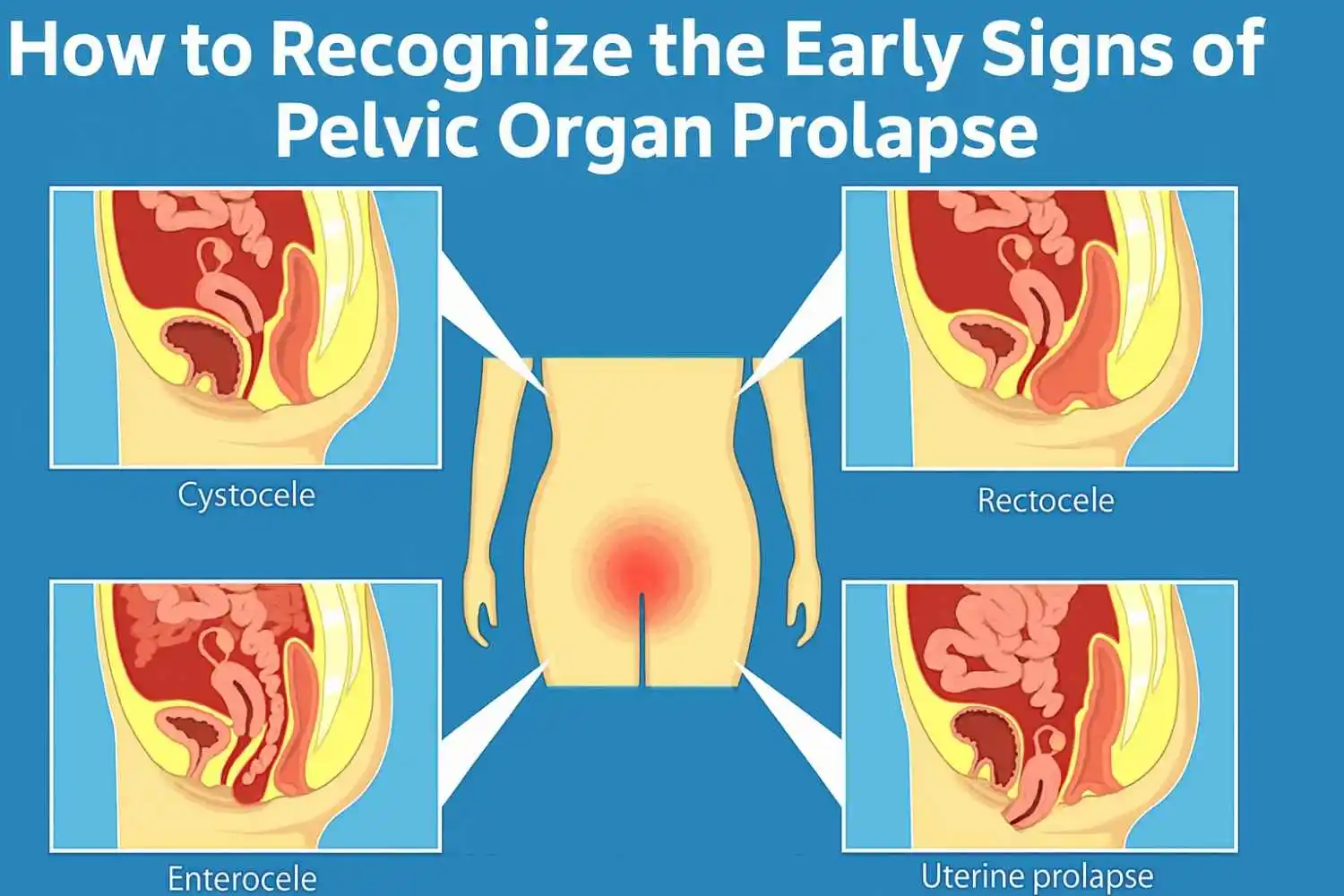
Rectal prolapse is a medical condition in which the rectum—the end of the large intestine—falls and protrudes through the anal opening. There is usually a visible red or pinkish bump at the anal opening that becomes more pronounced during and after a bowel movement. Essentially, the rectum appears to be inverting itself. Rectal prolapse may be startling to see, but it typically poses no immediate threat to life. Without early intervention, rectal prolapse can, however, lead to symptoms of pain, social embarrassment, or indirectly lead to complications that include faecal incontinence or prolonged chronic constipation.
Who is at risk? In the vast majority of cases, rectal prolapse is diagnosed in older adults, especially women who are older than 50. Women with a history of multiple vaginal deliveries or trauma while delivering babies may be at increased risk. Age-related weakening of the pelvic floor muscles, connective tissues, neurological conditions, and a history of untreated prolonged bouts of constipation can all contribute to a higher degree of risk for the development of rectal prolapse. Diagnosing rectal prolapse early on is key. Early identification of rectal prolapse means there are more options for effective, timely, and minimally invasive management of the condition. Treatment options include dietary changes and physiotherapy, as well as surgery that can greatly improve the patient's time and quality of life. Prompt medical intervention can help prevent complications such as strangulation of the rectal tissue, which cuts off blood supply to that tissue.
What is rectal prolapse?
Rectal prolapse manifests itself when the rectum (the final part of the large intestine) loses support and descends through the anal canal. It is a condition in which the rectum has “fallen” out of position, extending outside the anus.
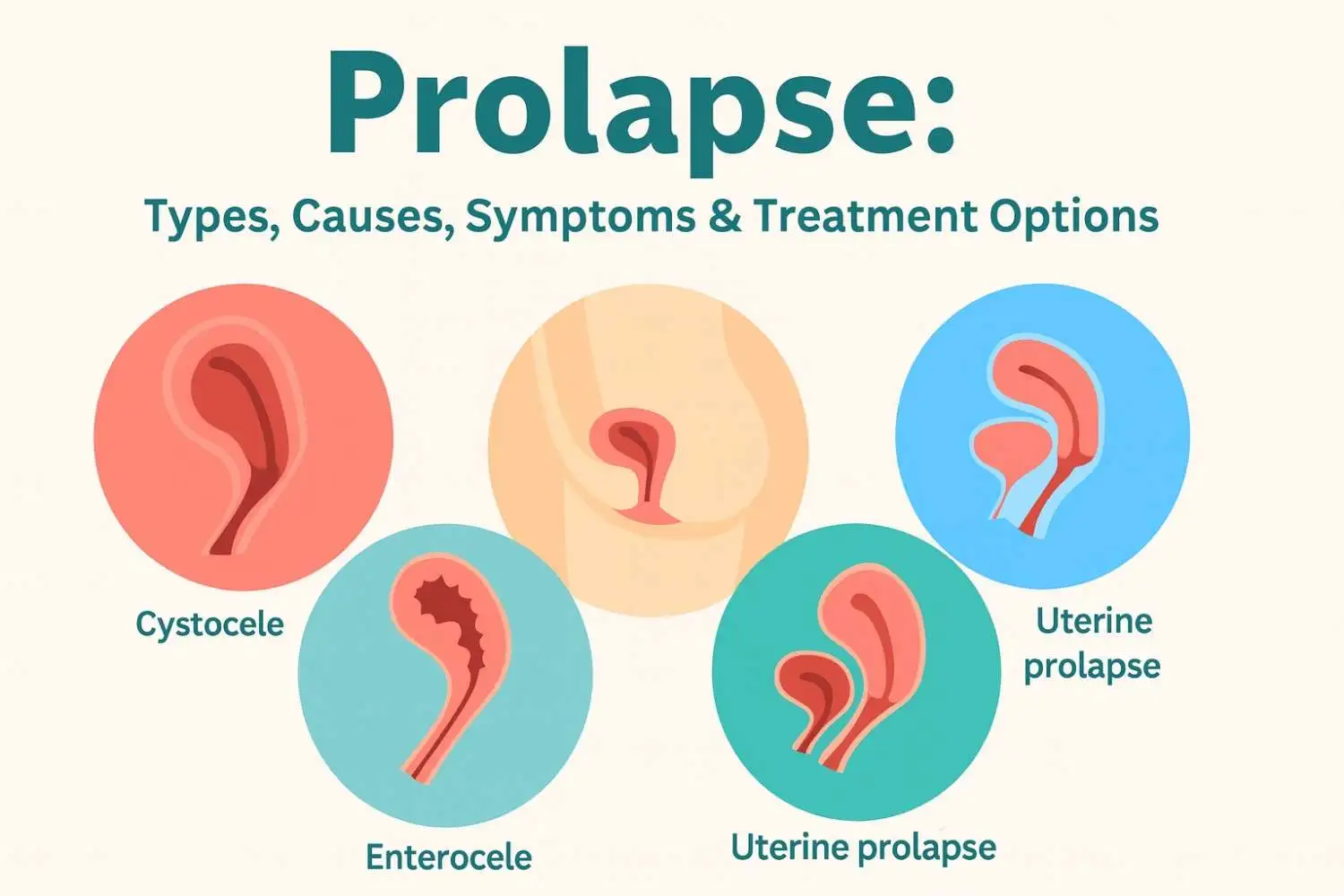
There are two basic types of rectal prolapse.
● External Prolapse:
The entire wall of the rectum protrudes through the anus and can be seen.
● Internal Prolapse (intussusception):
The rectum is folding into itself and is not protruding out of the anus.
There are also medical classifications of rectal prolapse:
● Mucosal prolapse:
Only the lining of the rectum protrudes.
● Complete (full-thickness) prolapse:
The entire wall of the rectum protrudes.
● Partial prolapse:
Only a segment of the rectum protrudes, usually just the mucosa.
Causes of Rectal Prolapse
Being aware of the causes of rectal prolapse will help you manage and even prevent this condition. Some of the most common culprits include:
● Chronic Constipation or Diarrhoea:
Straining repeatedly during bowel movements puts stress and strain on the rectum and pelvic muscles.
● Straining during bowel movements:
Often due to low fibre intake or poor toileting habits, but this straining can result in a rectal prolapse.
● Weakness of the Pelvic Floor Muscles:
Conditions such as pelvic floor dysfunction or problems caused by advanced age can play a significant role in weakness.
● Ageing:
Age decreases the elasticity and strength of tissues, which increases the chances of having a prolapse condition.
● Past Childbirth:
Especially women who have had multiple births, particularly vaginal deliveries. Childbirth can negatively impact pelvic muscles.
● Prior Surgery:
Previous pelvic surgeries may have weakened the connective tissue that supports the rectum.
● Problematic Neurological Conditions:
Neurological disorders that negatively impact nerve stimulus to muscles and surrounding tissue may also be reasons for pelvic floor dysfunction.
● Genetic Factors:
Some individuals may be born with or inherit connective tissues that are inherently weak.
● Chronic Coughing or Lifting:
Anything that raises pressure in the abdominal cavity can exert additional downward pressure that can push the rectum down following the weakening of connective tissues.
Rectal Prolapse Signs and Symptoms
Identifying the early indications of rectal prolapse symptoms is paramount if you want to get timely treatment options. Rectal prolapse can include the following symptoms:
● Visible Protruding from Anus:
This condition is often a reddish, fleshy protrusion from the anus during or shortly after a bowel movement.
● Feeling of Incomplete Bowel Evacuation after Bowel Movements:
Sometimes this feeling is present with the status of rectal prolapse.
● Rectal Bleeding or Mucus from Prolapse:
If the rectal tissues become irritated, you may see bleeding or mucus from the rectum, usually with a small degree of blood.
● Pain or Discomfort in or around the Rectum:
This pain may sometimes occur while sitting or during a bowel movement.
● Faecal Incontinence:
An inability to control bowel movements, usually associated with advanced-stage rectal prolapse.
But patients may also experience symptoms associated with rectal prolapse, with itching, constipation, or a feeling of pelvic pressure.
Rectal Prolapse Diagnosis
There are several ways to diagnose rectal prolapse, both physically and through imaging.
● Physical Exam:
The procedure involves visualisation and a digital rectal exam to assess anal sphincter tone.
● Colonoscopy/Sigmoidoscopy:
Used to rule out other possible complications (tumours, polyps).
● Defecography:
An X-ray is performed with a simulated bowel movement that looks at the movement of the rectum.
● MRI & Anorectal Manometry:
More advanced tests that evaluate muscle function and anatomic abnormalities.
● Endoanal ultrasound & EMG:
Used to assess the pelvic floor muscle's nerve supply and method of injury, if any.
All of these tools are helpful and necessary in determining whether we have an internal or external prolapse, as well as dictating the treatment pathway.
Rectal Prolapse Treatment Options
Depending on the severity of the prolapse, conservative management or surgical options can be explored.
1. Non-surgical Management
Dietary Adjustments: Increasing fibre intake (whole grains, fruits, and vegetables) can decrease episodes of constipation.
● Stool Softeners:
Decrease straining while having a bowel movement.
● Pelvic Floor Physiotherapy:
Check out our physiotherapy services and see how exercises can help.
● Biofeedback Therapy:
Improves the coordination of stressful pelvic floor muscles.
2. Surgical Options
Surgery is indicated for most moderate to severe degrees of rectal prolapse:
● Rectopexy:
Abdominal or laparoscopic procedure. The rectum is secured in place, preventing it from sliding downwards.
● Perineal operations:
These include the Delorme procedure. They are easier and safer to offer to patients who are elderly and at higher risk.
● Robotic Surgery:
Robotic surgery can provide surgical precision as well as quicker recovery in some patients with certain types of diseases.
The most appropriate treatment for rectal prolapse will depend on the patient's overall health, the type and severity of the prolapse, and their lifestyle.
Role of Physiotherapy in Rectal Prolapse
Physiotherapy is an excellent, non-invasive approach to treating, managing, and preventing rectal prolapse. Here are the ways it can help:
1. Pelvic Floor Muscle Strengthening:
Exercises such as Kegels and resistance training help strengthen the muscles that support the rectum.
2. Symptom Relief:
Physiotherapy can help relieve incontinence and discomfort in the pelvic area.
3. Post-surgical rehabilitation:
Physiotherapy helps to speed up recovery and reduce the recurrence of rectal prolapse.
Programs such as Pelvic Pain Dysfunction Therapy and Exercise & Pilates promote your core and pelvic health.
4. Complementary Approaches:
● Lifestyle and Dietary Changes: Eat high-fibre foods and hydrate.
● Take part in regular yoga, stretching, and walks.
5. Medical & OTC Options:
● Fibre supplements & laxatives (as prescribed).
6. Medication (prescription) for chronic constipation.
● Natural Remedies: Abdominal massage.
● Natural herbal teas (e.g., ginger).
● Probiotics improve gut flora.
Rectal Prolapse Prevention Tips
Here’s how to reduce your risk:
● Avoid Straining: Don’t force bowel movements.
● Eat a Fibre-Rich Diet: Include fruits, vegetables, legumes, and grains.
● Stay Hydrated: Drink 6–8 glasses of water daily.
● Do Regular Pelvic Floor Exercises: Strengthen muscles with Kegels.
● Treat Constipation Promptly: Prevent it from becoming chronic.
Avoid heavy lifting and maintain a healthy weight to reduce pelvic pressure.
When to See a Doctor for Rectal Prolapse
Seek medical help if:
● You notice a Bulge, especially during or after bowel movements.
● Persistent Incontinence or Constipation:
Could indicate underlying muscle or nerve issues.
● Pain or Bleeding:
During bowel movements, such discomfort requires immediate attention.
● You can’t push the Prolapse Back:
This procedure could lead to tissue strangulation.
● Heavy Bleeding or Fluid Discharge:
May indicate infection or other serious complications.
Prompt treatment ensures a better outcome and prevents escalation.
Conclusion
Rectal prolapse is manageable with early diagnosis and treatment. Whether that be through diet or lifestyle changes, physiotherapy intervention, or surgical treatment in more severe cases, recovery is achievable, and your standard of living can be returned to you.
If you or someone you know is experiencing the above symptoms, please reach out to a physician or our physiotherapy team. We would love to support you on your journey to pelvic health!
Frequently Asked Questions
Add comment






















.webp)





.jpg)






































