



.webp)
Author: Dr. Garima Biswas
Yoga 0
Dyspareunia, or painful intercourse, impairs the quality of life and emotional well-being of many people--most often women, but men can suffer, too. Dyspareunia is defined as "persistent or recurrent pain in the genital or pelvic region that occurs during or after sexual intercourse." The pain can be mild and infrequent for some people, while it occurs more often and is debilitating for many others. Dyspareunia not only affects the experience of intimacy but can also harm emotional closeness, well-being, and intimacy in a relationship.
It is important to resolve dyspareunia not only for physical health but also to improve emotional intimacy and relational harmony. Because of social taboos about discussing sexual dysfunction and the embarrassment it may evoke, the subject of dyspareunia for many people is rarely discussed, and they may suffer in silence. This silence also delays diagnosis and treatment, and some suffer prolonged physical pain, often accompanied by emotional distress and relationship discontent.
Although many people, and particularly women, will experience dyspareunia across the life span, it occurs more frequently during certain life stages, like menopause, post-childbirth, or after having undergone pelvic surgeries. But men are not exempt from dyspareunia; they, too, are known to experience dyspareunia for other reasons, including infections, skin disorders, or psychological stressors. Knowing what dyspareunia is, the causes of it, and the treatment options can help those affected find relief and regain control of their intimate health.
What is dyspareunia?
Dyspareunia means genital or pelvic pain felt during sex. Dyspareunia can be categorised based on where it is and what the pain feels like.
1. Superficial Dyspareunia:
Pain felt at the vaginal opening or tip of the penis during initial penetration. This type of discomfort is usually due to dryness, infections, or tightness of the muscles.
2. Deep Dyspareunia:
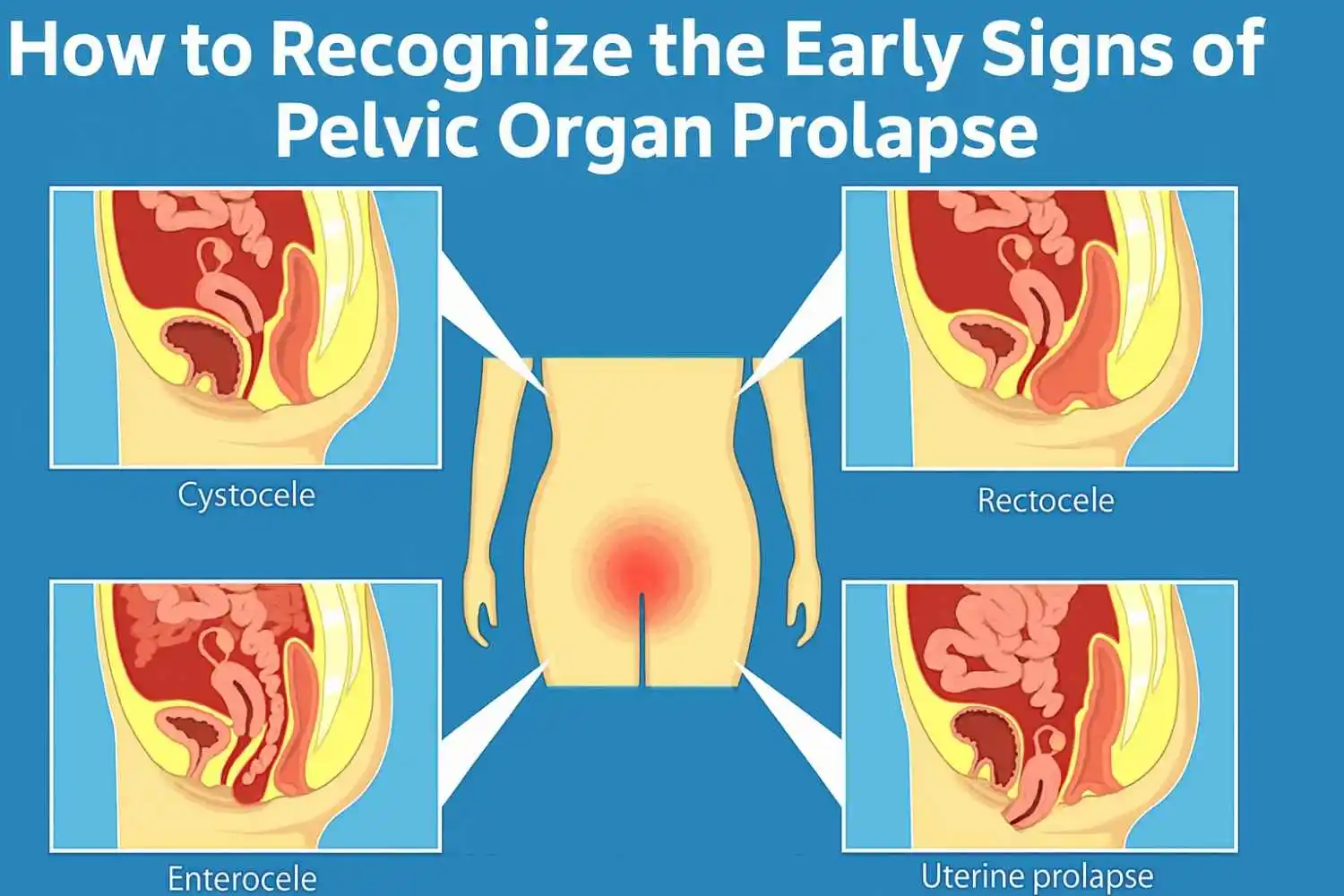
An internal condition like endometriosis, pelvic inflammatory disease, or ovarian cysts may cause pain during deeper penetration.
Dyspareunia symptoms can lead to physical distress and psychological problems, including fear of intercourse, anxiety, and relationship difficulties. And while dyspareunia primarily refers to physical pain, it also encompasses other aspects. It is the disruption of life and intimacy.
Causes of Dyspareunia
Determining the cause of dyspareunia is essential to treating it. There may be physical, psychological, or hormonal causes to consider:
1. Physical Causes:
a.Vaginal infections:
urinary tract infections, yeast infections, STIs
b. Endometriosis:
Abnormal tissue growth that generates deep pelvic pain (located in the lower abdomen) through the menstrual cycle, but can exist independent of a woman’s period
c. Vaginal dryness:
Sometimes will occur when a woman is going through menopause, when she is breastfeeding
● Pelvic inflammatory disease (PID)
● Vaginal atrophy or injury resulting from surgical procedures or childbirth
● Skin conditions, for example, lichen sclerosus
● Allergies to latex condoms, lubricants, or spermicides
2. Psychological Causes:
● Anxiety, or depression
● History of sexual trauma
● Relationship problems
● Negative body image
3. Hormonal Causes:
● Menopause leads to a decline in estrogen
● Contraceptive and antidepressant medications
● Diabetes or other endocrinological disorders
It is important to take a holistic view of the cause of dyspareunia when investigating causes because, generally speaking, more than one cause occurs concurrently.
Dyspareunia Common Symptoms
Symptoms of dyspareunia may range in severity as well as be sustained at multiple points during intercourse. The most common signs of dyspareunia include the following:
● Pain before, during, or after intercourse
● Burning, throbbing, or stinging sensations
● Discomfort during insertion or penetration
● Deep pelvic pain with thrusting
● Emotional symptoms like fear, avoidance, or distress about intimacy
These dyspareunia symptoms can often be confused with other conditions, which is why a precise diagnosis is crucial.
How is dyspareunia diagnosed?
Diagnosis of dyspareunia includes:
● Medical and sexual history:
Asking questions that will help relate the pain to its timing, location, and characteristics
● Pelvic examination:
To check for any visible objective signs of infection, trauma, or structural changes
● Infection tests:
Tests to determine whether there's evidence of STIs or yeast infections (e.g., swabs or cultures)
● Imaging tests:
Ultrasound or MRI to determine whether there are internal reasons (e.g., cysts, endometriosis)
● Referrals:
Depending on examination outcomes, our assessment may involve a gynecologist, urologist, or psychotherapist.
When dyspareunia is diagnosed accurately, targets can be achieved, resulting in positive health outcomes, including quality of life improvement.
Dyspareunia Treatment Options
Medical Treatments:
● Antibiotics or antifungals for infections
● Estrogen therapy for women post-menopause
● Topical anesthetics for pain relief
Pelvic Floor Therapy:
● Physiotherapy to relax and retrain pelvic muscles
● Vaginal dilators to stimulate and desensitize the vaginal tissues gradually
● Stretching and relaxation exercises
Psychological Support:
● Sex therapy to help rebuild intimacy and self-efficacy
● Cognitive Behavioral Therapy (CBT)
● Trauma counseling for women with a history of sexual abuse
Home Remedies & Lifestyle Tips:
● Use water-based lubricants
● Spend more time on foreplay
● Be comfortable communicating your specific needs to your partner
● Yoga and meditation for stress management
A personalised treatment plan that takes into account your dyspareunia meaning and specific symptoms is likely to produce positive results.
Dyspareunia in Men
Although less prevalent, men's dyspareunia is a real condition that merits consideration and may include:
● Infections such as prostatitis or urethritis
● Penile conditions such as Peyronie's disease or phimosis
● Skin lesions and conditions such as eczema or dermatitis
● Psychological stress or trauma
● Pain after ejaculation or discomfort with thrusting, and other potential conditions
Treatment may include antibiotics, counseling, or lifestyle changes. Knowing what dyspareunia is in men will help eliminate how society attaches stigma to gender.
When to Seek Help for Dyspareunia
Don't wait if:
● The pain is persistent or worsening.
● There is bleeding, fever, or discharge.
● It is causing emotional distress or strain on your relationship.
● You have been avoiding intimacy due to fear of pain.
See a gynaecologist, urologist, or sexual health therapist. Early intervention can help take control of your dyspareunia symptoms and help reclaim intimacy.
Dyspareunia Prevention Tips
While none of these are guarantees, the indicators below will help with further consideration:
● Be diligent about the hygiene of the genital parts.
● Use condoms to reduce STIs.
● Avoid chemical irritants such as scented soaps or lubricant products.
● Decrease stress with the help of yoga, meditation, or mental health support.
● Stay hydrated, and amp up foreplay practices.
● Schedule regular check-ups with a gynecologist or urologist
Check the list of strategies above to keep sexual health for both physical and emotional dimensions.
Conclusion
Dyspareunia is far more widespread than most people realize—and it is treatable. Whether the cause of dyspareunia is physical, emotional, or hormonal, reaching out for medical attention promptly and taking a multi-pronged approach to your treatment will help boost your outlook on life. Being open and empathetic and seeking professional medical care is essential in the healing process. If you or your partner has dyspareunia symptoms, act! Talk to someone, reach out, and take care of yourself!
Frequently Asked Questions























.webp)





.jpg)




































Subscribe now
Get the Latest
Updates With Our Newsletter

Copyright 2026 | Omansh.org
Website designed and developed by PulsePlay Digital

