




Author: Dr. Garima Biswas
WOMEN HEALTH 0
Vulvodynia is a chronic pain condition defined as vaginal pain, discomfort, burning, or stinging in the vulva that persists for three months or longer and has no identifiable cause. It is not a cancerous or infectious condition. Vulvodynia is a pain disorder of the vulva (female external genitals). Vulvodynia may impact a woman's quality of life significantly.
What is Vulvodynia?
Vulvodynia is a chronic pain condition of the vulva, the external female genitalia, defined as pain lasting three months or more and without an identifiable cause. Vulvodynia can cause burning, stinging, itching or soreness in the vulvar region. The pain can be localised or generalised (widespread), and it can impact a person's quality of life by affecting her ability to participate in things she enjoys, such as sitting for long periods of time or engaging in sexual activities.
Characteristics of Vulvodynia
● Persistent pain: the pain must last more than 3 months
● No identifiable cause: Unlike vulvar pain associated with infection or some cause, vulvodynia must have no identifiable cause.
● Pain can be burning, stinging, itching, and/or soreness
● Pain can impact a quality of life that is significant in terms of daily activities and relationships.
Symptoms of Vulvodynia
Vulvodynia is defined as a history of vulvar pain or discomfort of at least three months' duration without an identifiable cause. Common symptoms include burning, stinging, irritation, and rawness of the vulvar region.
Other symptoms could be:
●Itching:
While less common than the previously listed symptoms, some women may have itching.
● Aching:
A dull pain in the vulvar region.
● Soreness:
The vulva may be sore and tender to the touch.
● Throbbing:
There may be a pulsating problem in the vulvar area.
● Swelling:
The vulva may appear puffy or swollen.
● Burning:
A burning feeling in the vulvar region.
● Stinging:
A sharp pain which may occur and can be stimulated by touch or movement.
● Irritation:
A sore feeling or roughness of the vulva.
● Rawness:
The vulva may feel as though someone has scraped or rubbed it raw.
Additional Considerations:
● The pain can be localised to one specific area of the vulva or spread throughout the entire region.
● Vulvodynia can be triggered or worsened by certain activities, such as sitting for long periods, wearing tight clothing, or during sexual intercourse.
● The pain can have a significant impact on a woman's daily life, including sleep, concentration, and sexual relationships.
Vulvodynia Causes and Risk Factors
While researchers have not yet pinpointed exactly what causes vulvodynia (chronic vulvar pain), they have identified several potential causes or contributors. These potential causes include nerve dysfunction, inflammation, hormonal changes, and genetics. Risk factors regarding genital pain may include prior pelvic trauma or a history of infections and psychological thoughts that contribute, such as anxiety or depression, and are outlined in detail below.
Potential Causes & Contributors:
● Nerve Dysfunction:
Injury/irritation of the nerves in the vulva (including the pudendal nerve) may lead to vulvodynia.
● Inflammation:
There may be higher concentrations of inflammatory mediators in the vulvar tissue.
● Hormonal Changes:
Rapidly changing levels of estrogen (as in menopause) or changes due to hormonal contraception.
● Genetics:
There may be some genetic predisposition to a chronic pain condition, including vulvodynia.
● Pelvic Floor Muscle Dysfunction:
That there is a weakness or spasms of pelvic floor muscles leading to pain.
● Allergies or skin irritants:
Allergic reactions to chemicals or irritants applied to or used on the vulva may trigger worsening of vulvodynia.
● History of prior infections or trauma:
A history of past vaginal infections or urinary tract infections, or injury to the pelvis area, would give one a risk for vulvodynia.
● Psychological factors may also contribute to vulvodynia, such as anxiety, depression, or post-traumatic stress (PTSD).
Risk Factors:
● Age:
While vulvodynia can affect women of any age, it is more common in younger women.
● Ethnicity:
Certain ethnic groups may be more likely to experience vulvodynia.
● Comorbid Pain Conditions:
Women with other chronic pain conditions like fibromyalgia or interstitial cystitis may have a higher risk.
● Comorbid Psychological Conditions:
Those with anxiety, depression, or PTSD may be more susceptible.
Vulvodynia Diagnosis
Diagnosis of vulvodynia is a process of exclusion – meaning, healthcare providers will first rule out other possible causes of vulvar pain before diagnosing vulvodynia. Diagnosing vulvodynia involves taking a thorough medical history, performing a physical examination, and possibly performing other tests to rule out other vulvar conditions, like infections, dermatological conditions, or passive vulvar disorders.
Detailed diagnosis process:
-
Medical History:
The history will include a detailed complaint of the patient's vulvar pain, including the patterns of pain, location of pain, and how long the patient has been experiencing vulvar pain. The history will also encompass any symptoms that seem to trigger or are associated with the pain (e.g., dyspareunia, burning, itching, etc.).
-
Physical Examination:
A careful pelvic examination is completed, which includes a careful examination of the vulva and surrounding areas to check for anything unusual and noting the areas of tenderness.
-
Excluding Other Causes:
All of the tests and assessments may include cultures, biopsy specimens, or swabs, which would help detect possible infections, skin problems, or other vulvar disorders.
-
Cotton swab test:
The healthcare provider may use a cotton swab to map out the areas (domains) of discomfort, especially if vestibulodynia is suspected.
-
Pelvic Floor Assessment:
Lastly, the pelvic floor muscles will be assessed to examine if there is tenderness/dysfunction.
Important Considerations:
● Vulvodynia is often diagnosed when other potential causes of vulvar pain have been excluded.
● There are no specific laboratory tests for vulvodynia, so it relies on clinical assessment and ruling out other possibilities.
● The diagnosis of vulvodynia is a process, and it may take time to rule out all other conditions.
Vulvodynia Treatment Options
Vulvodynia treatment focuses on managing pain and improving quality of life, often involving a combination of approaches. The treatments may include topical medications like lidocaine, antidepressants, anticonvulsants, nerve blocks, physical therapy, and psychological support. In some cases, surgery may be an option.
Treatment Options:
● Topical Medications:
○ Local anaesthetics:
Creams or ointments like lidocaine can numb the vulva and provide short-term pain relief.
○ Hormonal creams:
Estrogen creams may help with pain and dryness, especially in post-menopausal women.
○ Anti-inflammatory creams:
Creams containing medications like amitriptyline, baclofen, or gabapentin can help manage nerve pain.
● Oral Medications:
○ Antidepressants:
Tricyclic antidepressants (TCAs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) can help reduce nerve pain and improve mood.
○ Anticonvulsants:
Medications like gabapentin and pregabalin can also help manage nerve pain.
● Nerve Blocks:
Injections of local anaesthetics or steroids can temporarily block pain signals from travelling to the brain.
● Physical Therapy:
○ Pelvic floor exercises:
Strengthening and relaxing pelvic floor muscles can reduce muscle spasms and improve pain.
○ Biofeedback:
This technique can help you learn to control your pelvic floor muscle tension and reduce pain.
● Psychological Support:
○ Cognitive Behavioural Therapy (CBT):
CBT can help you manage pain-related emotions, anxiety, and stress.
○ Psychosexual Therapy:
This type of therapy can address sexual dysfunction and improve sexual relationships.
● Surgical Options:
○ Vestibulectomy:
This surgery involves removing the painful tissue in the vestibule (the area around the vaginal opening).
● Other Treatments:
○ Acupuncture:
Some individuals find relief from acupuncture, which involves inserting thin needles into specific points on the body.
○ Hypnosis:
Hypnosis can help with relaxation and pain management.
○ Stress management techniques:
Practices like mindfulness and meditation can help reduce stress, which can worsen vulvodynia symptoms.
Living with Vulvodynia
Living with vulvodynia is not just a physical experience—it profoundly affects emotional, psychological, and social aspects of life. Since vulvodynia is a chronic condition, learning to manage it over time becomes essential to preserving overall well-being and quality of life.
Emotional Impact and Support
Chronic pain in intimate areas such as the vulva can lead to emotional distress. Women may experience anxiety, depression, and feelings of isolation, especially when the condition affects sexual relationships and day-to-day functionality. It's common for sufferers to feel frustrated or helpless, particularly if they faced delayed diagnosis or misunderstood symptoms.
Coping Mechanisms
● Medical management:
Pain relief through medications, pelvic floor physical therapy, and topical treatments can reduce physical symptoms.
● Pelvic floor therapy:
Regular exercises and relaxation techniques help address underlying muscular dysfunction.
● Mindfulness and stress management:
Techniques like yoga, meditation, and deep breathing exercises may improve mental focus and reduce the stress that often worsens pain.
● Biofeedback therapy:
This helps women gain control over involuntary body functions such as pelvic muscle tension, helping manage discomfort.
Support Groups and Counseling
Talking to others who understand your experience can be incredibly empowering. Support groups, either online or in person, provide emotional solidarity and practical advice. Cognitive Behavioural Therapy (CBT) and psychosexual therapy can help women navigate the emotional and relationship challenges of living with vulvodynia.
Open communication with partners and healthcare providers is crucial. Honest conversations can strengthen relationships and allow for tailored treatment plans that align with the patient's needs.
When to See a Doctor for Vulvodynia
Many women wait months or even years before seeking help for vulvar pain, often due to embarrassment or the misconception that it will resolve on its own. However, recognising when to consult a healthcare provider is crucial.
Signs That Require Medical Attention
● Chronic vulvar pain lasting more than three months
● Persistent symptoms such as burning, stinging, itching, or rawness
● Pain interfering with daily life including sleep, work, and sexual activity
● No improvement from self-care or over-the-counter treatments
Importance of Not Ignoring Chronic Pain
Ignoring symptoms of vulvodynia can delay diagnosis and prolong suffering. It can also affect mental health and relationships. Seeking help ensures early diagnosis and access to a wide range of treatment options, from topical and oral medications to physical therapy and counselling.
At your doctor’s appointment, expect a thorough history, physical examination, and possibly a cotton swab test to locate pain. Vulvodynia is a diagnosis of exclusion, meaning other causes such as infections, skin diseases, or STIs need to be ruled out first.
When to See a Doctor for Vulvodynia
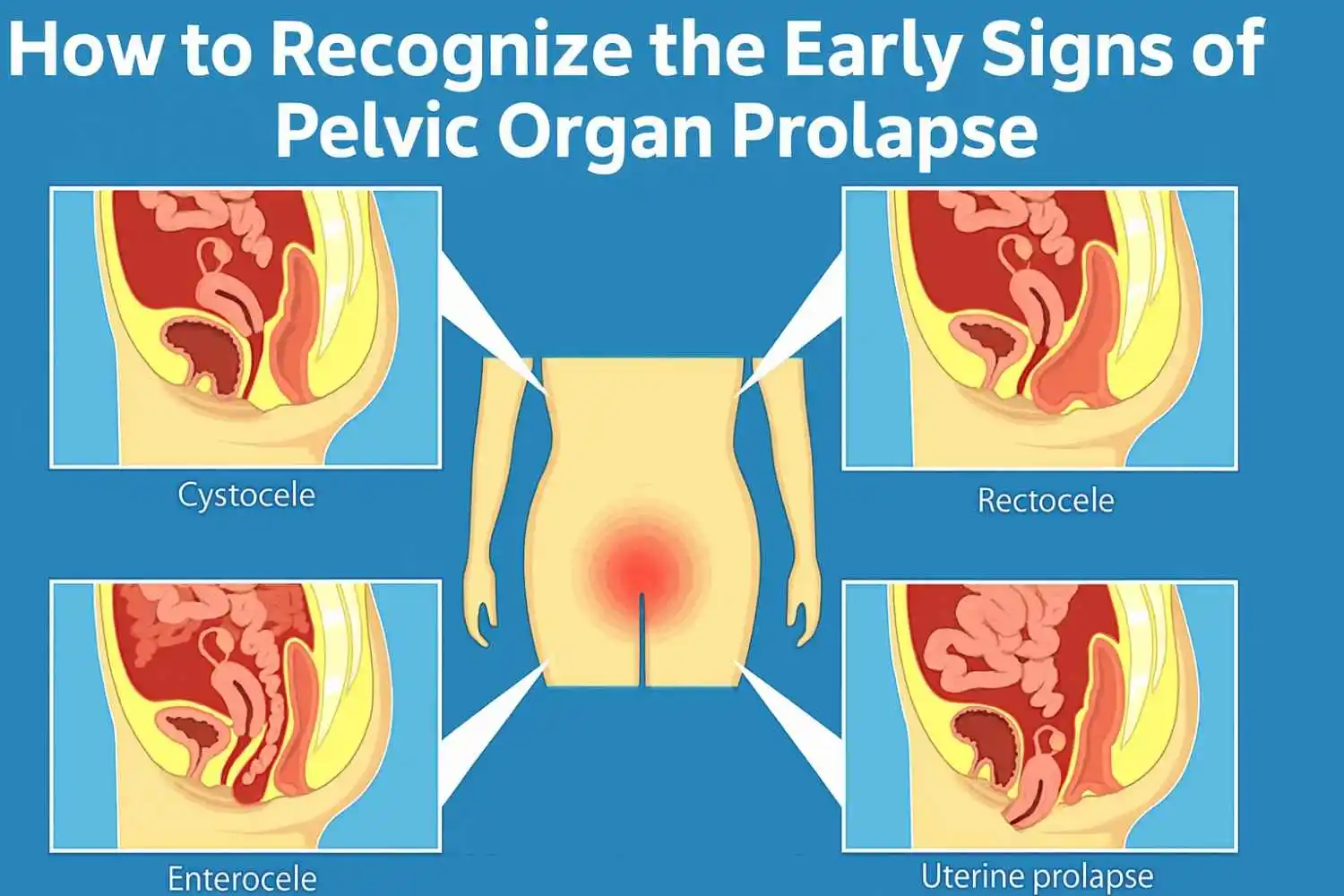
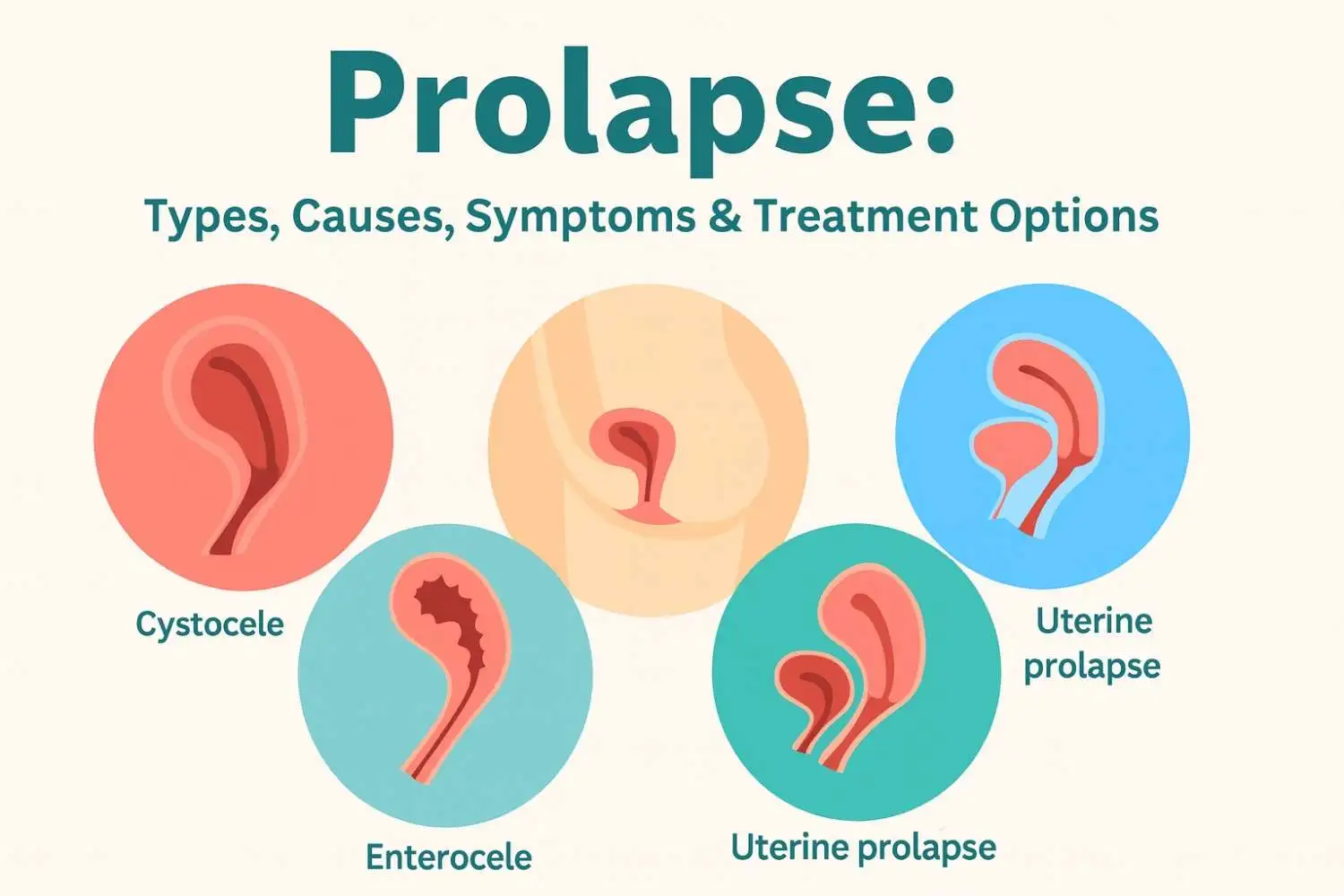
Though unrelated to vulvodynia, rectal prolapse is another condition involving pelvic health that requires prompt attention. Women, especially older adults or those with a history of chronic constipation, may experience this.
Key Warning Signs:
● A bulge from the rectum visible, especially after straining
● Persistent constipation or incontinence
● Pain or bleeding during bowel movements
● Inability to push the prolapse back in
Why seek medical help? Left untreated, rectal prolapse can lead to serious complications like tissue incarceration or blood supply loss. A doctor can confirm the diagnosis and recommend treatments—ranging from lifestyle modifications and pelvic floor therapy to surgery.
Conclusion
Vulvodynia is a complex, chronic pain condition that significantly impacts a woman's life—from physical comfort to emotional well-being. Recognising the symptoms early, understanding their potential causes, and exploring personalised treatment options are critical steps toward recovery.
Key Takeaways:
● Vulvodynia is not rare—but it is often underdiagnosed.
● Symptoms include persistent vulvar burning, irritation, and pain.
● Causes are often unclear but may include nerve irritation, hormonal changes, or psychological factors.
● Treatment is multi-faceted: medications, physical therapy, psychotherapy, and lifestyle changes.
● Support and empathy are essential. Women should be encouraged to speak up and seek the help they deserve.
At Omansh, we emphasise holistic pelvic health, which combines physiotherapy, lifestyle coaching, and mental wellness support. If you or someone you love is experiencing chronic vulvar pain, don’t hesitate to consult a healthcare provider or reach out to our expert team.
Frequently Asked Questions

























.webp)





.jpg)

































