



Author: Dr. Garima Bishwas
Yoga 0
Pelvic organ prolapse (POP) is more common than many women realize. It often goes undiscussed due to embarrassment or lack of awareness. But understanding the condition, its causes, symptoms, and treatments can empower women—especially those who are pregnant, postpartum, or managing pelvic health through physiotherapy or yoga—to take charge of their well-being.
What is Pelvic Organ Prolapse?
Pelvic organ prolapse occurs when the muscles and connective tissues that support your pelvic organs weaken, allowing one or more organs (bladder, uterus, vagina, rectum, or small intestine) to drop from their normal position. This descent often creates a bulge in the vaginal area and can lead to discomfort, pressure, or even visible protrusion.
Think of your pelvic floor as a hammock holding everything in place. When that support is compromised—due to childbirth, aging, or other factors—the organs may shift and sag.
Depending on the severity, some women might feel a minor pressure, while others may notice a bulge or something “falling out” of the vagina.
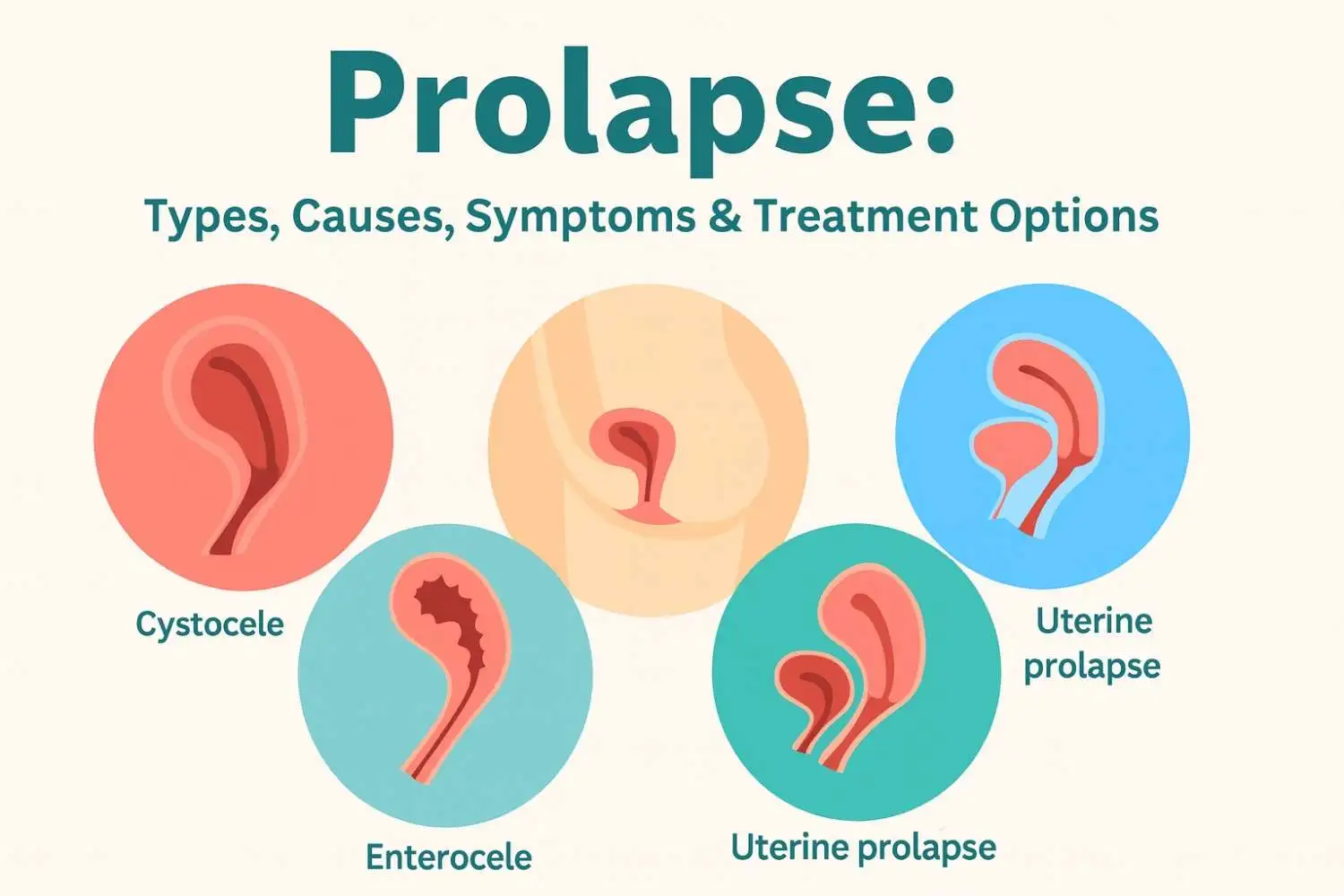
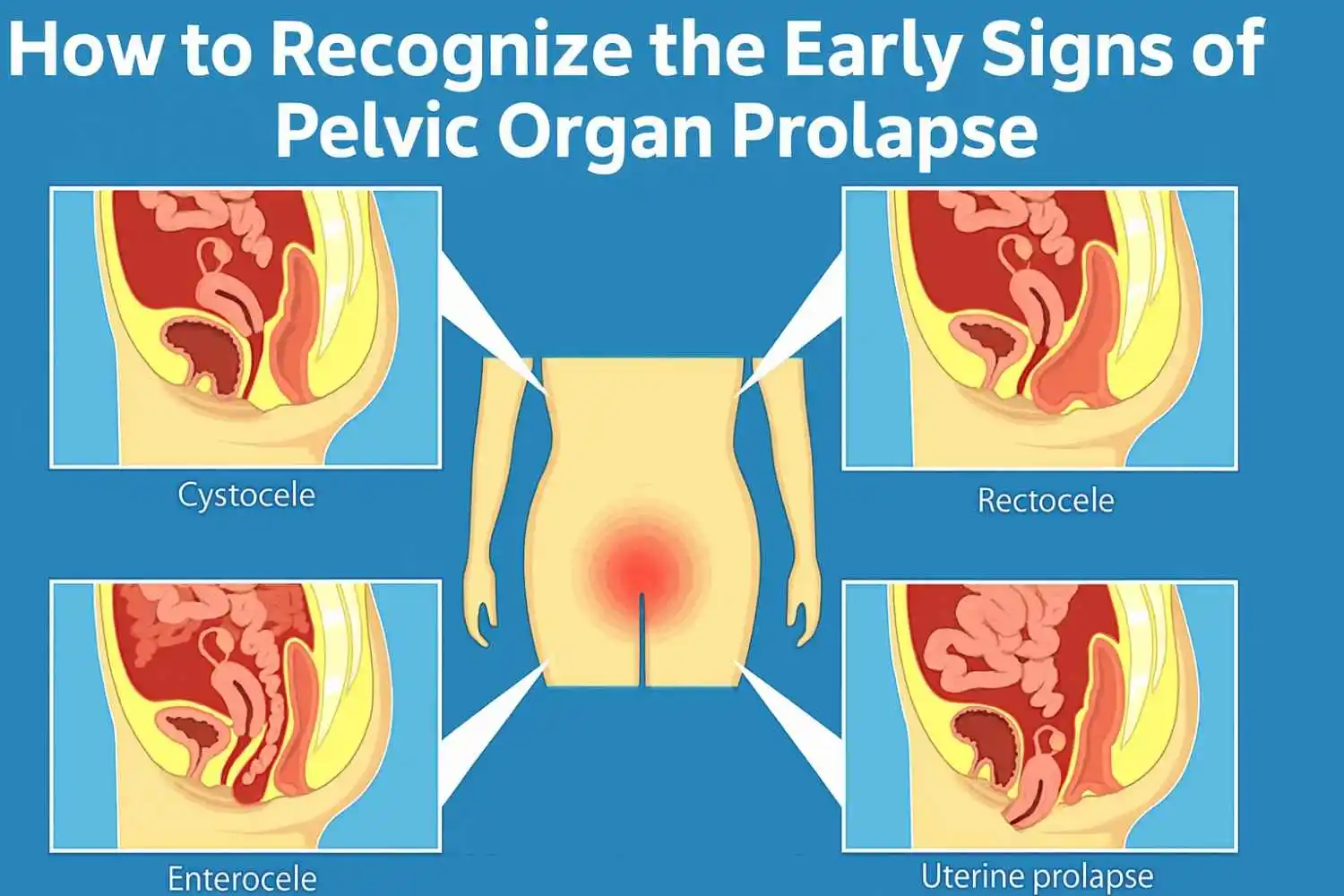
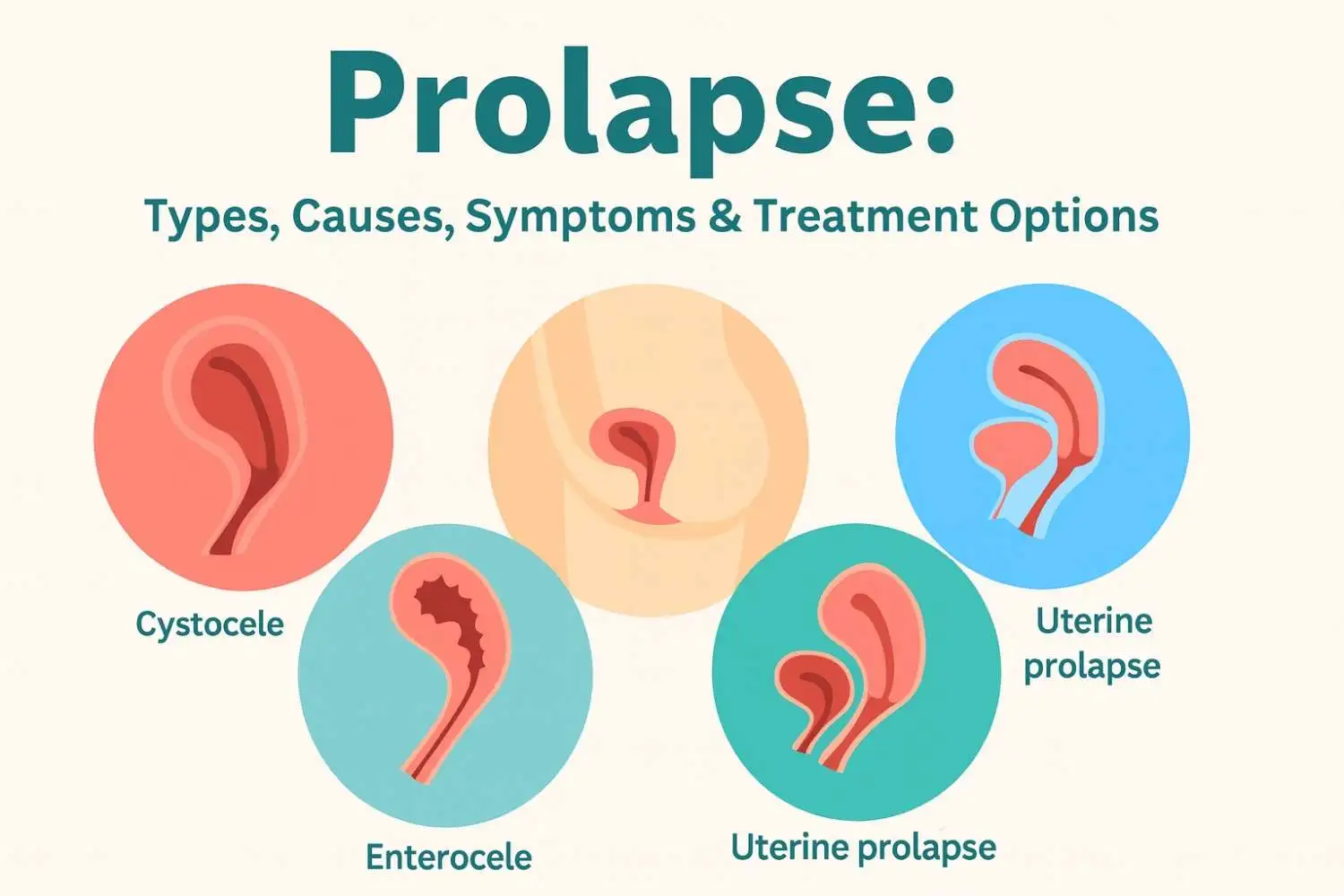
What Are the Different Types of Pelvic Organ Prolapse?
Pelvic organ prolapse isn’t a one-size-fits-all diagnosis. There are several types, depending on which organ is affected:
1. Cystocele (Bladder Prolapse)
When the bladder descends into the vaginal wall, causing pelvic pressure or urinary issues. You may feel a heaviness that worsens as the day progresses.
2. Rectocele (Rectum Prolapse)
The rectum pushes into the vagina, making bowel movements difficult or incomplete. Constipation and rectal pressure are common symptoms.
3. Uterine Prolapse
The uterus drops into the vaginal canal. In severe cases, it may protrude outside the vagina.
4. Enterocele
This involves the small intestine falling into the vaginal space, often after a hysterectomy.
5. Apical Prolapse
Occurs when the top of the vagina descends, especially after the uterus has been surgically removed.
These types may occur separately or together and vary from mild to severe.
What Causes Pelvic Organ Prolapse?
Several risk factors contribute to weakening the pelvic floor:
1. Childbirth
Vaginal deliveries, particularly those involving prolonged labor, large babies, or assisted tools (forceps/vacuum), stretch or tear pelvic tissues.
2. Aging
With age, muscle tone decreases, especially after menopause due to reduced estrogen, which supports connective tissue health.
3. Obesity
Extra weight increases abdominal pressure, placing more strain on the pelvic floor.
4. Chronic Straining
Long-term constipation, heavy lifting, or chronic coughing can overstress pelvic muscles.
5. Connective Tissue Disorders
Some women have genetically weaker connective tissues, making them more susceptible to prolapse.
6. Hysterectomy
Removing the uterus can disrupt the natural support system of pelvic organs.
7. Hormonal Changes
Estrogen decline post-menopause weakens tissues, increasing prolapse risk.
What Are the Common Symptoms of Pelvic Organ Prolapse?
Symptoms vary based on the type and severity but often include:
-
A feeling of pelvic pressure or fullness, like something is “falling out”
-
Visible or palpable bulge in or outside the vagina
-
Urinary incontinence or trouble fully emptying the bladder
-
Bowel movement issues, like constipation or straining
-
Pain during intercourse or decreased sensation
-
Lower back pain and groin discomfort
-
Difficulty using tampons or menstrual cups
These symptoms may worsen after standing, lifting, or a long day of physical activity.
How Is Pelvic Organ Prolapse Diagnosed?
Your healthcare provider will conduct a comprehensive evaluation:
1. Medical History
They’ll ask about childbirth, surgical history, urinary or bowel problems, and sexual health concerns.
2. Pelvic Examination
During this manual exam, you may be asked to cough or strain, revealing any bulging or descent. The POP-Q system is often used to measure and stage the prolapse.
3. Additional Tests
-
Bladder function tests (urodynamics) for incontinence
-
Bowel studies for rectal involvement
-
Imaging (MRI or ultrasound) for complex or multi-organ prolapse
A complete diagnosis ensures a tailored treatment plan.
What Are the Treatment Options for Pelvic Organ Prolapse?
Treatment depends on your symptoms, prolapse severity, age, and personal goals (e.g., future pregnancies).
1. Conservative Treatments:
a. Pelvic Floor Exercises (Kegels)
These are first-line interventions. They strengthen the pelvic muscles, improving mild symptoms and preventing worsening.
b. Vaginal Pessary
A silicone device inserted into the vagina to hold organs in place. Useful for those avoiding or not ready for surgery.
c. Lifestyle Changes
-
Weight loss
-
High-fiber diet to manage constipation
-
Avoid heavy lifting
-
Quit smoking to protect connective tissue and reduce coughing.
2. Surgical Treatments:
a. Reconstructive Surgery
Restores normal organ placement. Can be done vaginally, laparoscopically, or abdominally.
b. Obliterative Surgery
Closes part of the vaginal canal, suitable for women not planning to remain sexually active.
c. Surgical Mesh
May provide support in some cases but carries risks. Always discuss FDA warnings and alternatives with your surgeon.
Can Pelvic Organ Prolapse Be Prevented?
While not 100% preventable, you can significantly reduce your risk with the following strategies:
1. Regular Kegel Exercises – Engage your pelvic muscles daily.
2. Maintain a Healthy Weight – Less pressure on your pelvic floor.
3. Avoid Heavy Lifting – Use proper techniques if necessary.
4. Manage Constipation – Eat fibre-rich foods and hydrate.
5. Treat Chronic Coughs – Avoid repeated strain on your core.
6. Quit Smoking – Smoking deteriorates tissue health.
7. Posture and Core Strength – Yoga and physiotherapy can support alignment and reduce stress on the pelvic region.
How Can I Live With Pelvic Organ Prolapse?
Living with POP means managing symptoms and making small but effective daily changes.
-
Kegels can make a big difference if done consistently and correctly (consult a pelvic floor therapist).
-
Eat fiber-rich meals and drink enough water to prevent straining.
-
Engage in low-impact exercises like yoga or walking.
-
Use supportive devices like pessaries when recommended.
-
Consider pelvic health physiotherapy for guided rehabilitation.
At Omansh, we advocate gentle, regular yoga and physiotherapy programs focused on pelvic health for long-term management.
When Should You See a Doctor for Pelvic Organ Prolapse?
Seek medical advice if:
-
You feel vaginal pressure or bulging
-
You struggle with urination or bowel movements
-
You experience sexual discomfort
-
Symptoms are affecting your lifestyle or mental health
Early intervention can prevent worsening, improve comfort, and expand your treatment options.
Expect your doctor to conduct a pelvic exam and may refer you to a urogynecologist, a specialist in female pelvic medicine.
Is Surgery Always Necessary for Pelvic Organ Prolapse?
No. Many women manage mild to moderate prolapse without surgery.
Surgery is considered when:
-
Conservative treatments aren’t enough
-
The prolapse is severe or interferes with daily life
-
There are complications like incontinence
Discuss all your options with your provider. Your choice should reflect your lifestyle, health status, and preferences.
Frequently Asked Questions (FAQs)
1. What is pelvic organ prolapse?
A condition where pelvic organs drop into or outside the vagina due to weakened pelvic floor support.
2. What are the types?
Cystocele, rectocele, uterine prolapse, enterocele, and apical prolapse.
3. What causes it?
Childbirth, aging, obesity, chronic straining, and more.
4. What are the symptoms?
Vaginal bulging, pressure, urinary or bowel issues, and sexual discomfort.
5. How is it diagnosed?
Via medical history, pelvic exams, and sometimes imaging or functional tests.
6. What are the treatment options?
Pelvic floor exercises, pessaries, lifestyle changes, and surgery in severe cases.
7. Can it be prevented?
Yes, through Kegels, weight management, avoiding heavy lifting, and more.
8. How to live with POP?
With lifestyle modifications, medical support, and pelvic floor strengthening.
9. When to see a doctor?
When symptoms interfere with daily life or cause discomfort.
10. Is surgery always necessary?
No. Many cases are managed non-surgically.























.webp)





.jpg)




































Subscribe now
Get the Latest
Updates With Our Newsletter

Copyright 2026 | Omansh.org
Website designed and developed by PulsePlay Digital

