



Author: Dr. Garima Bishwas
Yoga 0
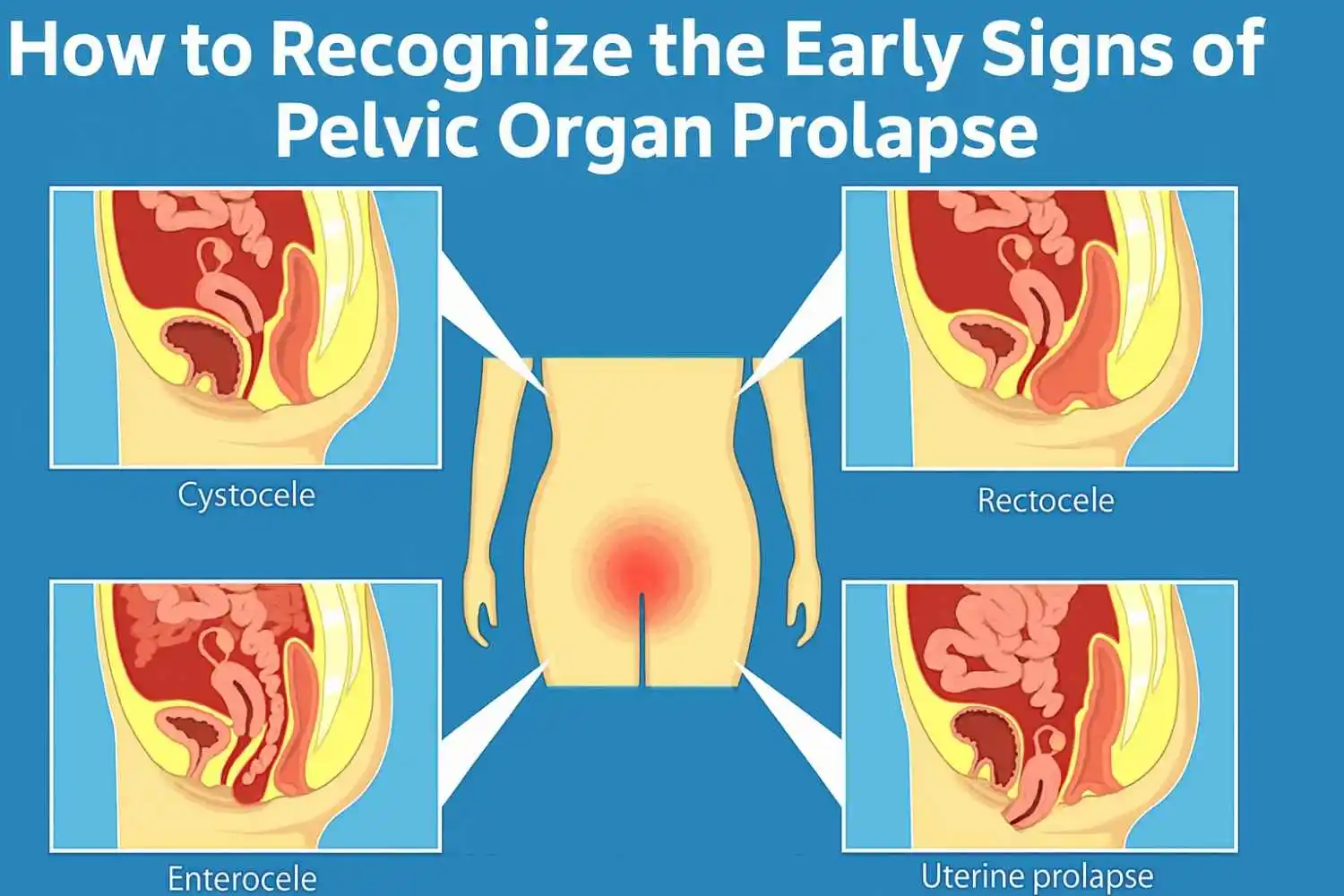
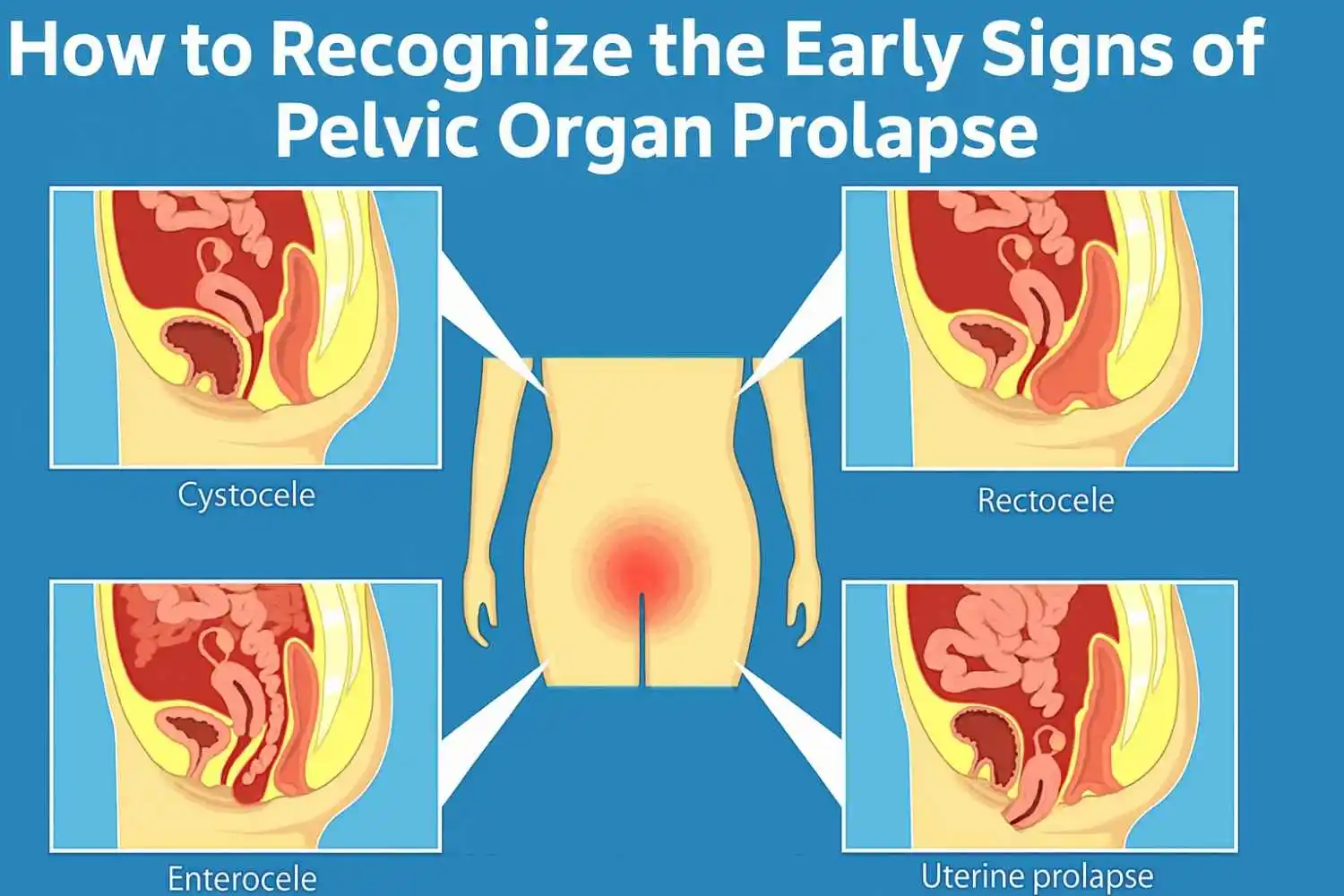
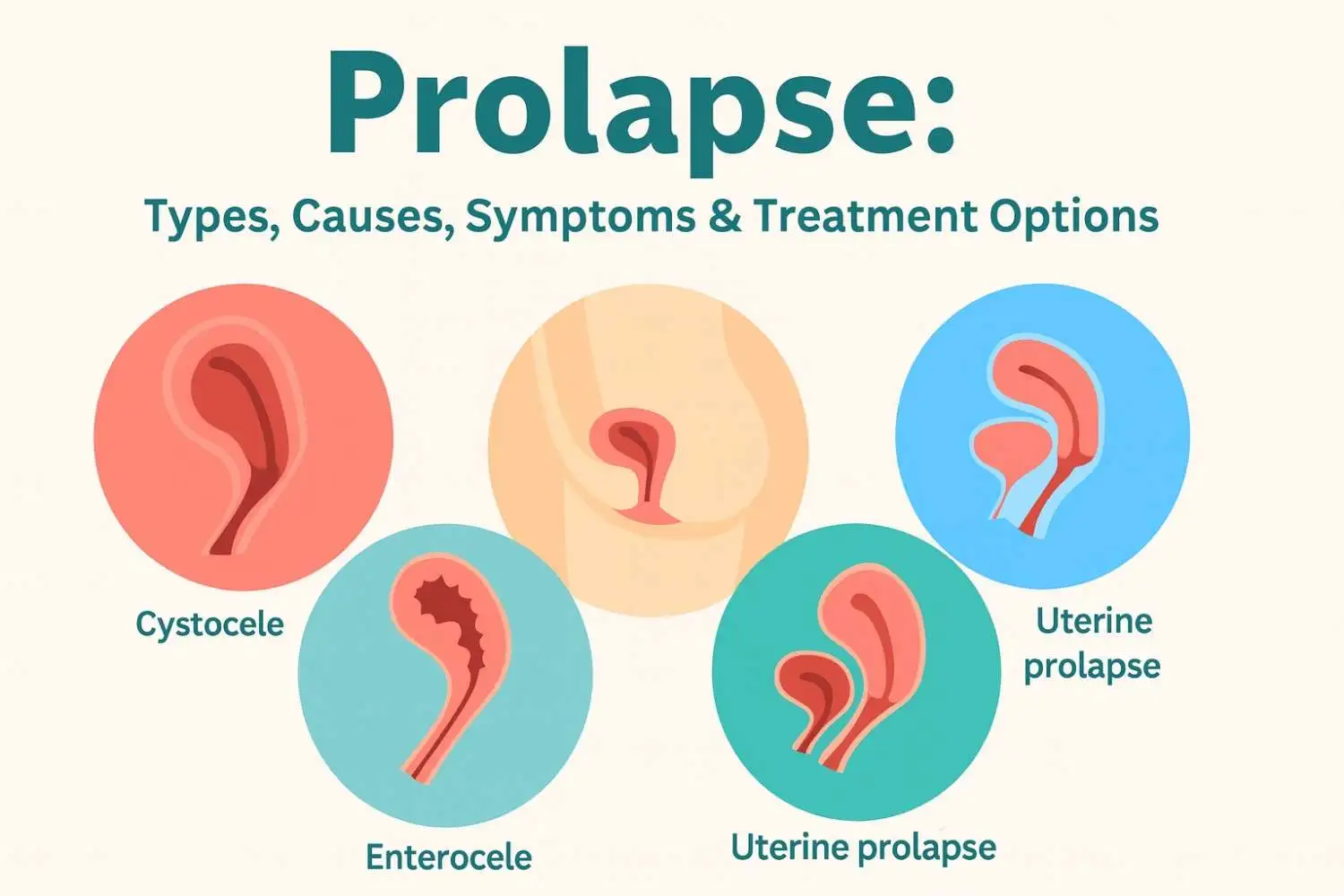
Pelvic Organ Prolapse (POP) is a condition where one or more of the pelvic organs - such as the bladder, uterus, or rectum - drop from their normal position and push against the walls of the vagina. This happens when the pelvic floor muscles and tissues become weak or stretched.
Who is commonly affected?
Pelvic organ prolapse primarily affects women, especially those who have given birth vaginally. It is more common in postmenopausal women and those with a history of heavy lifting, obesity, or chronic constipation.
Why Early Detection of Pelvic Organ Prolapse Matters
Recognizing the early signs of pelvic organ prolapse is crucial for timely intervention and avoiding complications. Here's why early detection is important:
1. Prevents Progression
If left untreated, mild prolapse can worsen over time, potentially leading to severe symptoms and the need for surgical treatment.
2. Improves Quality of Life
Addressing early signs like pelvic pressure or incontinence can enhance daily comfort and enable more active participation in life.
3. Reduces Need for Invasive Procedures
Mild cases are often managed through non-invasive treatments like pelvic floor exercises, pessaries, or lifestyle changes. Early management may eliminate the need for surgery.
4. Prevents Complications
Severe prolapse may lead to urinary tract infections, kidney issues, and emotional strain. Early treatment can help prevent these outcomes.
5. Promotes Better Outcomes
The earlier the treatment, the higher the likelihood of successful symptom relief and long-term management.
Common Early Signs and Symptoms to Watch For
Spotting the early signs of pelvic organ prolapse can make a huge difference in preventing further deterioration. Here are some of the most common symptoms:
1. Sensation of Heaviness or Pressure in the Pelvis
You may feel like something is pulling or dragging in the pelvic area. This sensation often worsens after standing for long periods, exercising, or coughing.
2. A Bulge or Lump in the Vagina
One of the clearest early signs of pelvic organ prolapse is feeling or seeing a bulge in the vaginal area, especially during activities like lifting or after a bowel movement.
3. Discomfort During Bowel Movements or Urination
Urinary and bowel symptoms, such as incomplete emptying, constipation, or leakage, are early indicators of POP.
4. Lower Back Pain Without Other Cause
Persistent lower back pain, especially when not related to physical strain or injury, may be linked to prolapse.
5. Vaginal Dryness or Discomfort During Intercourse
Pain or dryness during sex could signal that the vaginal structure has been altered due to prolapse.
6. Difficulty Using Tampons
If tampons no longer stay in place or feel uncomfortable, this may indicate a change in vaginal anatomy associated with early POP.
Important Considerations:
-
Symptoms may fluctuate and differ from woman to woman.
-
Even mild symptoms warrant medical attention to rule out or confirm POP.
If you're experiencing pelvic pressure or a vaginal bulge, it may be a sign of prolapse. Learn more about pelvic organ prolapse symptoms and treatment.
Pelvic Organ Prolapse Risk Factors That Make Early Signs More Likely
Understanding what increases your risk can help you recognize early signs of pelvic organ prolapse before it progresses.
1. Childbirth History
Multiple vaginal deliveries, large babies, or the use of forceps/vacuum increase the chance of pelvic muscle strain, a major contributor to POP.
2. Age and Menopause
As estrogen levels decline post-menopause, pelvic tissues can weaken, increasing vulnerability to prolapse.
3. Obesity or Heavy Lifting
Excess weight and repeated heavy lifting place pressure on the pelvic floor muscles, raising the risk.
4. Chronic Coughing or Constipation
Long-term coughing or straining during bowel movements stresses the pelvic muscles, contributing to their weakening.
5. Genetics and Connective Tissue Disorders
If you have a family history of prolapse or conditions like Ehlers-Danlos syndrome, your risk may be higher.
When to See a Doctor
Don't ignore symptoms, especially if they affect your daily life. See a healthcare provider if you notice:
-
A visible bulge or feeling of something falling out of the vagina
-
Persistent pelvic pressure or discomfort
-
Pain during intercourse
-
Urinary or bowel changes
How is POP diagnosed?
A gynecologist or urogynecologist will perform a pelvic exam and may use imaging tests like an ultrasound or an MRI to assess the severity.
Pelvic Organ Prolapse Self-Checks & At-Home Awareness Tips
While not a substitute for medical evaluation, self-checks can help you stay in tune with your body:
1. Self-Check Techniques:
-
Observe: Use a mirror to look for any visible bulging at the vaginal opening.
-
Feel: With clean hands, gently insert a finger to detect any unusual lumps.
-
Note: Pay attention to when pelvic pressure feels more intense (e.g., after standing or lifting).
-
Monitor: Keep a symptom diary to track when signs appear or worsen.
2. At-Home Awareness & Prevention:
-
Diet: High-fiber foods and hydration help prevent constipation.
-
Bowel Movements: Avoid straining and allow time for natural elimination.
-
Weight Management: Maintain a healthy body weight to ease pressure on the pelvis.
-
Heavy Lifting: Use proper lifting techniques, exhaling during effort.
-
Manage Cough: Treat chronic coughs and consider quitting smoking.
-
Posture: Practice upright posture to reduce intra-abdominal pressure.
-
Pelvic Floor Exercises: Kegel exercises are especially helpful for strengthening internal support.
-
Professional Guidance: Consult a pelvic health physiotherapist or doctor for tailored advice.
Final Thoughts
Pelvic organ prolapse may begin subtly, but recognizing and responding to the early signs of pelvic organ prolapse can make all the difference. Don’t dismiss symptoms like pressure, discomfort, or urinary changes as "just aging" or "normal after childbirth."
Taking early action leads to better outcomes, preserves quality of life, and may prevent the need for surgical intervention. If you have concerns, speak with a healthcare provider and explore your options - your pelvic health matters.
Frequently Asked Questions























.webp)





.jpg)




































Subscribe now
Get the Latest
Updates With Our Newsletter

Copyright 2026 | Omansh.org
Website designed and developed by PulsePlay Digital

